C is the correct answer
Explanation:
This question is not only testing your knowledge about the effectiveness of different over-the-counter medications for nasal congestion but also whether you’ve been listening to the news lately. In September, the FDA held an advisory committee meeting to discuss the lack of effectiveness of phenylephrine, an alpha-1 receptor agonist, for short-term congestive symptoms. The advisory committee concluded that phenylephrine is ineffective in its current dose, but there are no safety concerns. Now, the FDA will consider this advisory decision and decide whether to remove phenylephrine from the market.
Phenylephrine has been studied for nasal decongestion for over 50 years. Its use became more popular when similar decongestants, like pseudoephedrine, were being misused in methamphetamine drug labs.
Ephedrine, an alpha- and beta-adrenergic agonist, is a compound that has been used since antiquity, and studies on pseudoephedrine began in the 1920s. Merck was the first company to produce and market ephedrine and pseudoephedrine, and over time, such agents have become popular to reduce nasal congestion related to viral upper respiratory tract infection (URI) and allergic rhinitis.
However, researchers and clinicians started to raise alarm bells about the lack of effectiveness of phenylephrine in 2007. Experts indicate that phenylephrine works no better than a placebo in treating nasal congestion, though the low dosage has made it a safe drug, especially in patients at risk for stroke and cardiovascular disease. Now the evidence has become overwhelming that phenylephrine in over-the-counter doses does not provide relief of nasal congestion, yet it is packaged and sold in numerous single and combination therapies.
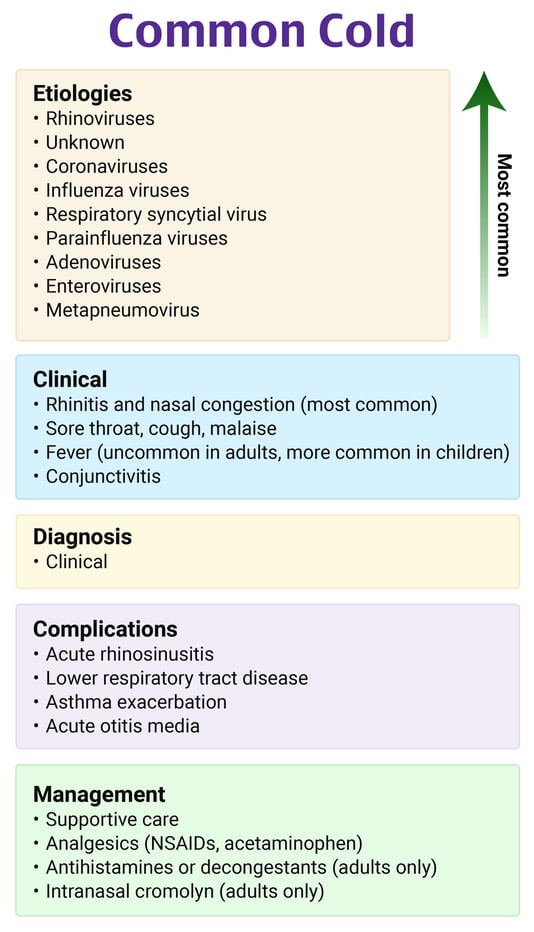
There are several ways to attempt to treat nasal congestion with over-the-counter medications:
- - Phenylephrine
- - Pseudoephedrine
- - Antihistamines (loratadine, diphenhydramine, cetirizine)
- - Topical oxymetazoline
- - Topical steroid spray (fluticasone)
- - Humidifier
- - Nasal adhesive strip
- - Menthol gel
- - Neti pot
None of them work wonderfully. The evidence surrounding the effectiveness of these different options is also incredibly challenging to analyze, largely due to the heterogeneity of studies, different study populations (allergic rhinitis versus viral URI), and the use of combination medications with pain relievers and other cough suppressants. Essentially, any benefit that has been found (antihistamines, oxymetazoline, pseudoephedrine) is small. However, the evidence seems more consistent in that phenylephrine pretty much does nothing over a placebo.
You can review a bunch of literature options yourself, as several of them are included in the references below.
The literature analysis does not blow one away to recommend pseudoephedrine, oxymetazoline, or antihistamines (like diphenhydramine) for nasal congestion, but here is a quick summary:
- - Oxymetazoline and pseudoephedrine both improve congestive symptoms, but oxymetazoline works much faster
- - While congestion in the short term improves with oxymetazoline and pseudoephedrine, most people do not report an overall feeling of wellness sooner when taking the medications
- - More recent evidence indicates that, among these options, oxymetazoline is probably the most effective
- - An antihistamine combined with a decongestant more often shows effectiveness over placebo
- - An antihistamine combined with an analgesic is sometimes effective
- - An antihistamine with an analgesic and a decongestant is more often effective in several studies (five out of six studies)
However, even though the adverse effects are often mild, none of these medications are without side effects. Oxymetazoline has the risk of rebound congestion if it is used for too many days. Oral pseudoephedrine should be avoided in patients who have risks for coronary artery disease, severe hypertension, and stroke. Antihistamines can be sedating, but this is more often when they are combined with other medications like dextromethorphan.
From this information, it is challenging to recommend a perfect medication for nasal congestion, but you can rest assured that the one you should not tell people to take is phenylephrine. When giving patients advice about symptom management for viral URI, consider the line I use: “Buy the stuff from behind the counter, not in front of the counter.”
References:
- Deckx L, De Sutter AI, Guo L, Mir NA, van Driel ML. Nasal decongestants in monotherapy for the common cold. Cochrane Database Syst Rev. 2016;10(10):CD009612.
- DeGeorge KC, Ring DJ, Dalrymple SN. Treatment of the common cold. Am Fam Physician. 2019;100(5):281–289.
- De Sutter AI, Eriksson L, van Driel ML. Oral antihistamine-decongestant-analgesic combinations for the common cold. Cochrane Database Syst Rev. 2022;1(1):CD004976.
- FDA clarifies results of recent advisory committee meeting on oral phenylephrine. U.S. Food & Drug Administration website. Accessed September 21, 2023.
- Gelotte CK, Zimmerman BA. Pharmacokinetics, safety, and cardiovascular tolerability of phenylephrine HCl 10, 20, and 30 mg after a single oral administration in healthy volunteers. Clin Drug Investig. 2015;35(9):547–558.
- Laccourreye O, Werner A, Giroud JP, Couloigner V, Bonfils P, Bondon-Guitton E. Benefits, limits and danger of ephedrine and pseudoephedrine as nasal decongestants. Eur Ann Otorhinolaryngol Head Neck Dis. 2015;132(1):31–34.
- Meltzer EO, Ratner PH, McGraw T. Oral phenylephrine HCl for nasal congestion in seasonal allergic rhinitis: a randomized, open-label, placebo-controlled study. J Allergy Clin Immunol Pract. 2015;3(5):702–708.
- Ng CC, Romaikin D, Steacy LM, et al. Comparative nasal airflow with loratadine-pseudoephedrine and fluticasone nasal spray for allergic rhinitis. Ann Allergy Asthma Immunol. 2021;127(3):342–348.e2.
P.S. Want to test your knowledge with more questions like this? Take advantage of 15% off the Rosh Review Scholar EM Qbank. You'll get 25 new questions with detailed explanations + images and 50 CME annually!
Use code: RebelEMScholar

