D is the correct answer
Explanation:
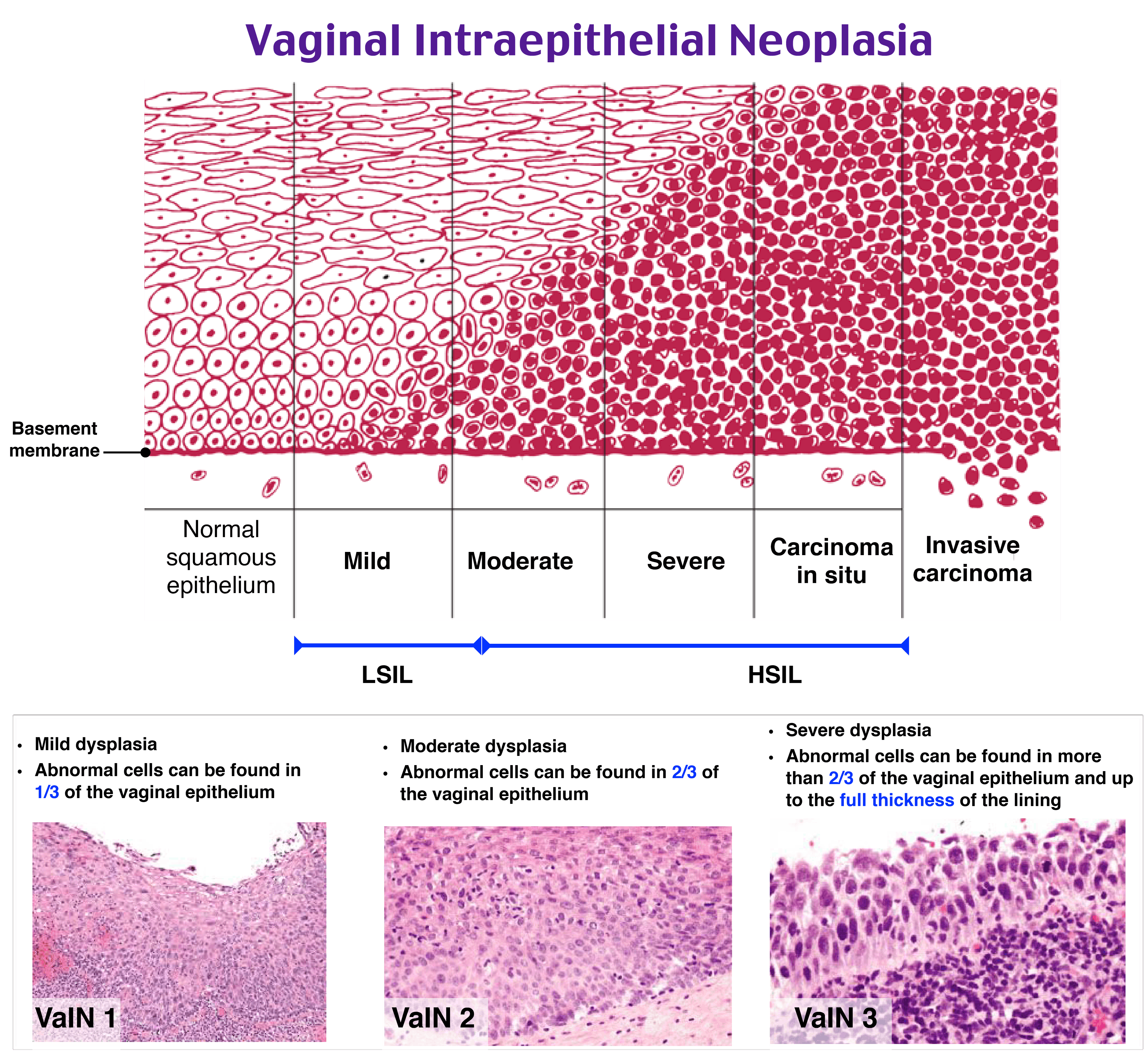
Vaginal intraepithelial neoplasia (VaIN) resembles cervical intraepithelial neoplasia (CIN) both by risk factors, pathophysiology, and appearance on histology. Similarly to CIN, exposure to human papillomavirus (HPV), particularlyHPV 16 or 18, is the leading cause of VaIN. Other risk factors include immunodeficiency and smoking. VaIN should be excluded in patients with abnormal cytology after a total hysterectomy, or those who present with postcoital bleeding or abnormal vaginal discharge, not explained by cervical etiologies.
A vaginoscopy with directed biopsies helps to differentiate low-grade disease from high-grade disease. In the setting of high-grade disease which is not completely visualized on vaginoscopy, surgical excision is preferred because it allows for histologic examination of the specimen to rule out focally invasive disease. A partial vaginectomy may be required when VaIN is buried in posthysterectomy suture recesses.
CO2 laser ablation (A) is not appropriate in this patient because all lesions were not completely visualized and invasive disease has not been ruled out. The presence of high-grade lesions is a result of human papillomavirus infection. Human papillomavirus vaccination (B) is used to prevent, not to treat, neoplastic lesions. Imiquimod (C) has been demonstrated in a meta-analysis to be as effective as laser ablation for the treatment of VaIN. However, topical imiquimod therapy would not be appropriate in this patient because invasive disease has not been excluded.
P.S. Want to test your knowledge with more questions like this? Take advantage of 20% off the Rosh Review CREOG Qbank and get access to 2,000 CREOG-formatted questions with detailed explanations and images!

